As ‘lockdowns’ and other restrictions are starting to ease in many countries, an awful lot of people seem to think this marks the beginning of a gradual return to ‘normal’.
Think again. Biology doesn’t work like that. We haven’t ‘beaten’ this virus; far from it. Restrictions on movement don’t change an organism; it’s the same as it was at the start of all this. It’s still highly contagious and – for many – remains very dangerous.
Social distancing and other such restrictions do not make pandemic viruses go away, they just help ‘flatten the curve’ so that we don’t overwhelm health systems and so contribute to preventable excess deaths.
But flattening the curve has other benefits too. It gives us some space to learn more about the little bugger and, sure enough, we now have far more data showing what the risks are – and aren’t.
I’ll return to that in a minute, but just to stick with going back to ‘normal’ for a moment, the natural history of this organism (and the natural history of large-scale novel outbreaks) dictates that the risk of infection from this will persist for some considerable time. This means the likely ‘new normal’ involves society and industry repeatedly going in and out of lockdowns at a national, regional, or even a community level.
In many places the restrictions have been sufficiently effective at bringing R0 down that – rather predictably – idiots are saying it was all an overreaction, there’s nothing to worry about and they ‘want their freedoms back‘. Incidentally, these are the same people who take an assault rifle to the grocery store in case the yoghurt looks at them funny.
Yes, we do have to accept that it’s not feasible to switch off global economic activity indefinitely but it’s not binary: it’s also not feasible to go straight back to ‘business as usual’.
To extend Boris Johnson’s analogy that “we can see light at the end of the tunnel – but we’re still in the tunnel”, the point is this is not the only tunnel.
It’s likely to be the first of several (if not many) and we’ll be in and out of them until well over half the population has developed immunity, either through exposure or vaccination. And that depends on a bunch of factors which is a whole other load of posts.
[It depends on the level of natural immunity that results from an infection, how long it will take to create a vaccine and how protective that vaccine will be and while the positive results from using convalescent sera as a treatment bode well, we’re a long way off yet. As I say, that’s a whole other can of worms I’m trying to resist in this post]
The nature of these things is the virus is likely to reappear in waves lasting many weeks at time, depending on the severity and the extent of any further lockdowns adopted.
Lessons About Spread
There is a bunch of stuff we’ve learned since this all started which can inform how we can manage risk both socially and in the workplace. It’s been clear for a while that – after accounting for age distribution and pre-existing health issues – risk of infection and mortality clearly splits between two groups: those in densely crowded areas – and everyone else.
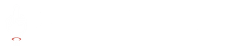
Large, densely populated areas like London and New York saw nearly twice the rate of transmission in the first two weeks of their respective outbreaks compared with more sparsely populated areas.
Coronavirus numbers are looking MUCH better, going down almost everywhere. Big progress being made!
— Donald J. Trump (@realDonaldTrump) May 11, 2020
New York is interesting in that the sheer scale of the outbreak hugely skews the US numbers. The graph above from this New York Times article shows the effect the NYC cases have on the overall US numbers and it’s dramatic. If you split the graph into two – NYC and everywhere else – it’s clear the trend is still upward in the rest of the US.
I’ll look at why calls by the Tangerine Shitgibbon to designate all places of worship – including churches, synagogues and mosques – as “essential,” and wanting them “open right now” is so mind-numbingly ill-informed and dangerous in a bit. First a brief crash-course in basic virology terms and numbers.
Virology in Numbers
There’s a couple of key terms and concepts to understand. I’ll keep it brief. It’s not complicated.
Where 'Social' Distancing Fails
So, if someone with it is sneezing into a small space and producing 40,000 droplets per sneeze, that’s more virus in the air than that person just breathing. Studies on flu have shown an infected person just breathing is releasing something like 25-50 virus particles per minute. Talking releases more, coughing releases more still, singing releases a lot too.
This is where we run into the limitations of social distancing. Social distancing only helps with brief or outdoor exposure to the virus, where there’s either insufficient time to take in an infectious dose, or where wind and space dilute any virus present (as well as the UV in sunlight zapping it).
Social distancing when applied to an office or a restaurant or a sports or entertainment venue doesn’t really work, as is now apparent in the data as you’ll see below.
Risk is Indoors, Not Outdoors
It’s becoming increasingly apparent that most if not all of the spread happens inside buildings. There have been ‘superspreader’ events in churches, auditoria and elsewhere and a recent paper out of China looking at 318 outbreaks across 120 cities involving over 7,000 cases found all identified outbreaks involving three or more cases occurred in an indoor environment.
That paper awaits peer review but it’s certainly not alone in suggesting sharing indoor space is a major contributor to infection risk: another paper out of Japan showed the chance of a primary case transmitting COVID-19 in a closed environment was nearly twenty times greater than in the open air.
One of the most interesting findings is from the CDC in South Korea – who are held in high regard given the way the outbreak was managed there. They recently investigated an outbreak in a call centre in Seoul and tested 1,143 people. They found 97 confirmed cases and of these 94 were working in an 11th-floor call centre. The blue colour shows where confirmed cases were sitting.
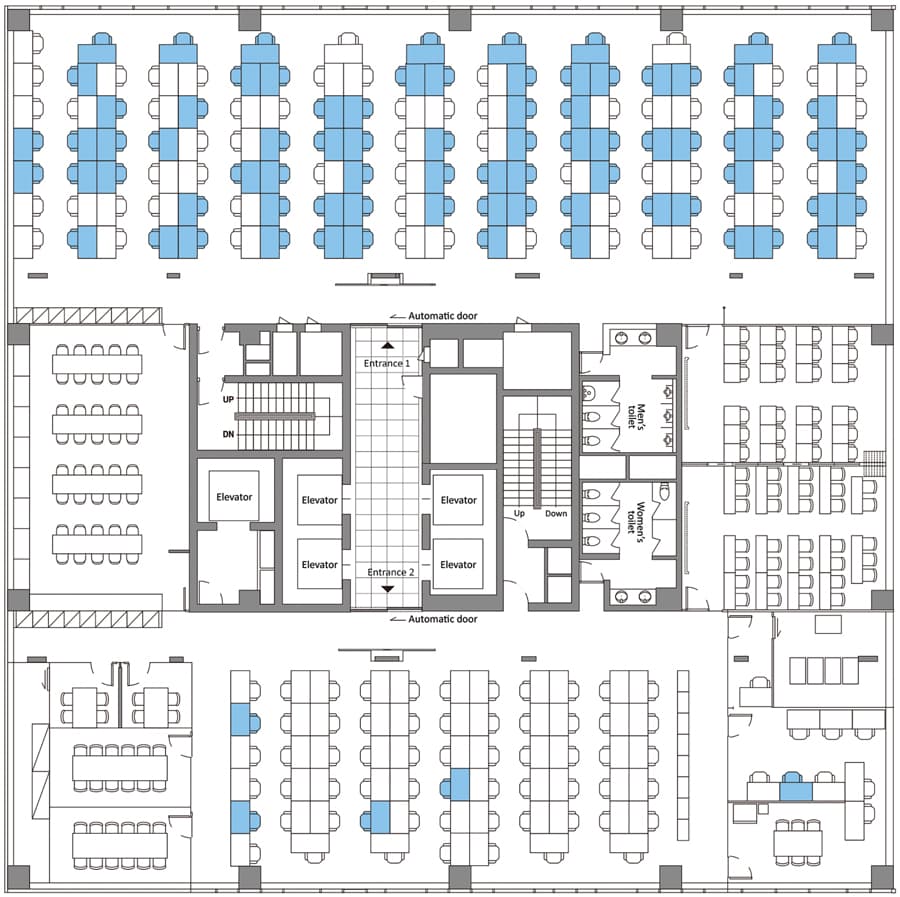
The paper makes interesting reading and shows the benefits of extensive contact tracing and testing – but for me, the really interesting aspect is it suggests the virus does not spread so easily via fomites (surfaces).
Were it spreading via high-touch surfaces, more people in that building would have been sickened by touching lift buttons, door handles etc. The outbreak was almost entirely limited to one call centre in one part of one floor where staff were in close proximity. It didn’t spread via high-touch surfaces or in lobbies, washrooms etc.
These are not the only examples. Careful contact tracing has shown there have been outbreaks originating in restaurants and many from religious events of all flavours – there have been examples in Korea, Israel, Iran, plus it seems communal singing is a culprit. There have been a number of choirs where it spread like wildfire with very high attack rates.
There are now sufficient studies showing this really is a droplet-borne ‘social’ virus that the US CDC changed its advice yesterday.
What does this mean for our social and working lives? It’s apparent physical distancing won’t be enough, especially indoors; it’s droplet control too.
The 3Cs Model
While it’s very difficult to compare countries as there are so many confounding factors the Japanese model or “Three Cs” (when translated from mitsu no mitsu) is interesting. The advice is to avoid closed spaces with poor ventilation, crowded places with many people nearby and close-contact settings such as close-range conversations.
But in Japan mask-wearing is far more widespread anyway and behaviours like shaking hands, embracing and other forms of physical contact are not part of traditional Japanese greetings. Also conversing on crowded commuter trains is considered poor etiquette – and using a mobile is even worse. These behaviours all help limit the possibility of droplet transmission; as I say comparisons are difficult but the 3Cs message fits in well with the emerging data.
AVOID
Closed SpacesClosed Spaces
AVOID CLOSED SPACES WITH POOR VENTILATION
AVOID
Crowded PlacesCrowded Places
AVOID PLACES CROWDED WITH MANY PEOPLE
AVOID
Close ContactClose Contact
AVOID CLOSE CONTACT SUCH AS CLOSE-RANGE CONVERSATIONS
Social Gatherings
I really can’t see a return to large-scale sports events, concerts or religious events anytime soon. At least not in countries that place the importance of public safety higher than that of collective acts of religious observance (be they of the sporting or god-bothering variety).
Here in the UK it’s been suggested almost twice as many people visit the theatre every year in London as watch Premier League football but I’m not hopeful for either. At least football matches could be played to empty stadia if the economics are viable – but the same really can’t be said of theatres. Ditto the 170 million cinema visits per year.
While considering the arts (rare for a philistine like me) I think it’s brighter for film and TV production though, pretty much all of which bar news is currently suspended and desperate to get back to work. And everyone on lockdown is relying on them for new content! Yes, these are complex workplaces but they are still workplaces. And in workplaces risks can be (and are required to be) assessed and managed.
This is an industry where every activity is risk-assessed, so this is another one to add to the list – but very much in the light of current data. It’s probably critical they take really good advice from experts in infection control rather than just Health and Safety too; I can’t think of many industries where you might be spending millions on a drama shoot and if the talent gets sick you’re finished. Will it require changes to the way things happen? Of course it will, especially if you need to produce content at anything like the same pace as before.
This is a good example of needing to understand where the risks actually are rather than guessing and for that you need microbiologists or infection control experts. H&S people are lovely but I’ve seen many examples recently of non-experts take ‘model’ procedures from elsewhere and try to turn them into a workplace policy. It’s seldom pretty.
Returning to Work
I’m parking issues of mental health, legal and safety requirements for employers – I’m a microbiologist, remember?
For businesses contemplating bringing staff back from remote working or furlough, the modelling above makes it clear it’s not so much common touchpoints, it’s common airspaces that presents the principal risk. I’m not suggesting we give up sanitising touchpoints – far from it – but workplaces need to recognise the level of risk now associated with people talking for hours in close proximity – often with inadequate ventilation.
- At work it’s not so much about social distancing, it’s about physical barriers – screens and cubicles – rather than open offices and the 3Cs. Masks alone won’t cut it (see later).
- Meetings will need to be the exception – and if they are absolutely necessary they need to be shorter and smaller.
- Strategies for cohorting / separating teams could help.
- Visibly sanitising touchpoints etc might not be the most critical intervention in the light of the above data – but make staff feel safer which is very important.
But if you get the airflow/ventilation part wrong, people will get sick no matter how often you wipe the door handles. It’s all in the data…
Care is required, though – when considering ventilation note that in the restaurant example earlier overenthusiastic aircon above one table blew respiratory droplets across multiple diners.
In some regards, the advice remains the same. Distancing, not touching your face, and washing / sanitising your hands are the key interventions at an individual level. Wearing gloves is not helpful; the virus does not get in through the skin and may increase your risk because you likely won’t wash or sanitise your hands when they are on plus you’ll be touching stuff.
But at an organisational level, it’s much more about managing air spaces and ventilation.
Answers
Overall, what this means is we all need to accept some level of risk – but that’s an individual as well as a collective decision. Someone who is aged and with poor lung health will likely make very different choices to someone who’s younger and otherwise healthy.
Irrespective of any future containment/lockdown strategy this is not going away any time soon.
We’re talking years, not months – so shutting down the economy, education and everything else until it goes away really isn’t an option. Because it’s not going away.
We have to learn to live with it and do whatever we can to mitigate risk. But individuals and organisations need to properly understand the risk or they can’t manage it.
Again, in a workplace social distancing in the sense most people understand it will not offer the protection you think it does. Anway, to sum up:
Where's the Risk?
If you’re outside and you walk past someone, even if they have it for any likelihood of picking it up you’d likely need to be in close proximity for a number of minutes for any chance of an infection to spread. While joggers or cyclists may be releasing more virus due to deeper breathing, the exposure time is tiny as they zoom past. Yes, maintain a distance but don’t get paranoid; the risk is vanishingly small.
If you’re in a large supermarket or shopping mall you need to consider the volume of the space (large?), the number of other people (most likely restricted?), how long you’re spending there (half an hour?) and if you’re in a well-ventilated, large space with not too many people, the risk is low.
But if you’re working there the risk is higher – the extended time provides a greater chance of getting an infectious dose – risk = amount of virus exposure x exposure time, remember? Also in such environments staff are likely seeing many customers / others so the risk is higher. It’s a numbers game.
Basically you need to look at each environment you’re going to be in and make judgements. How many people? How much ventilation? How long will you be there? If you’re in an open office the assessment is more critical (volume of the space, people, and ventilation) – and if people are talking face-to-face the risk increases.
But most of all, your best strategy for mitigating risk is to listen to expert advice. And that advice WILL change as we discover more. Listen to infectious disease experts and reputable sources. And remember that reputable sources and proper scientists do not publish ‘research’ exclusively via YouTube videos.
Most of all, don’t listen to a science-denying serial lair who bribed a porn star in a conspiracy to conceal an affair they conducted while his third wife was giving birth to his child when he tells you how important it is for churches to reopen so YOU can all pray more.
Just sayin’…
Masks Post Script
Just a final word on masks – which also deserve a whole post. There are many types of mask, many ways of measuring effectiveness and many conflicting studies. If you have a particular bias or preconception about whether to use a particular type of mask in a particular situation you will be able to find a study that supports your hunch quite easily – as well as an equal and opposite study showing your bias is wrong.
You could be forgiven for thinking the potential benefits of mask wearing are so face-palmingly obvious, the simple fact they have not been made mandatory is proof positive of Government incompetence. But this is biology. It’s complicated. Sorry. I know everyone wants it all to be simple but it’s not.
The evidence and utility in healthcare settings where N95 or similar masks are being used by people trained to wear them properly and not touch their faces, or by people actively shedding virus is a very different proposition to wearing a mask on public transport or in an office.
While I’ve not been a fan of people who aren’t showing symptoms wearing masks (especially the types of mask needed by healthcare workers that have been in short supply) my view is evolving. But slowly.
There was a recent paper in Nature about surgical (as opposed to N95) masks that said:
“surgical face masks could prevent transmission of human coronaviruses and influenza viruses from symptomatic individuals”
The results weren’t stellar (like most studies into this) hence the pretty wishy-washy conclusion. Most studies show masks may be of some benefit in terms of preventing wearers both spreading or receiving the virus – but the data says the benefit is likely to be very modest. They offer nothing near ‘full’ protection – far from it.
The biggest factor in terms of non-medical use of face masks is how people actually use them. The studies show that the modest decrease in risk of spread is only there if people use their masks consistently and properly. When they don’t, what little protection there is vanishes.
And most people don’t use masks properly: they don’t fit them correctly, they keep adjusting and touching them and there’s now good data showing the extent of virus deposition on the outside of face masks, so if you have it touching your mask is a really good way to spread it. There’s also the false sense of security issue (just as there is with gloves) – people may well not be as rigorous with social distancing when wearing a mask just as people get lax with hand hygiene when wearing gloves.
So don’t overestimate the benefits and stick to the stuff (like hand and respiratory hygiene) that’s proven to work. If you absolutely have to wear one make sure you’ve had training so it actually protects you and others. I’m still trying to get my head around what this will look like for mass transit when capacity returns. Leave that with me for now…



So we’re all doomed Sean Derrig
Tony – yes, we’re all going to die. Just not necessarily of COVID…
Sean Derrig I know – off to the hospital for an out patients appointment – the charming lady I’ve been trading wound photos with assured me last week 67 is the new 40 so I’m ok then ….
Keep well Chap
Just when we thought it was safe to venture out!?!
Good piece, thanks!
Great piece!
My husband refused to wear mask while working…in forest. ;-)
People here wear home-sewn cotton masks like in Japan 40 years ago…any tips?
A lone worker in a forest? Difficult to think of a lower-risk environment. Tell him Bat Soup is off the menu for now, though. Masks? The Japanese example is a good one; it’s not just the masks, it’s culture too – the lack of physical contact generally when greeting and the other stuff I mentioned above that has a huge input. Mitsu-desu!
The use of common sense .protect yourself .keep your distance .
Caroljean Horton no thanks I have an immune system
Sue G. Darton 👍 you are a lucky one .
Caroljean Horton not really. We’re all born with one normally
Sue G. Darton 👍
Did anyone else read that as rectal fossil?
What a load of bollocks, it’s never been proven that viruses even exist, it’s a Scamdemic and your trying to make money off the back of it, thank God Trump’s on the job
Paul Hindley Da, Tovarishch.
Paul Hindley I think you need to see a psychiatrist! So how do you explain all these deaths?
Sandra Docherty I don’t need anything and I’ll say it again, it’s never been proven that viruses even exist and that’s just a fact
Al Freeman, got a good one here!
The brainwashed believe proven liars, has everyone forgot about the 6 illegal wars the Tory and Labour party started ? Millions of totally innocent men women and children murdered in our name and not one shot fired at us first and you people believe them about this Scamdemic, lol
Chris Fairbrother no you have someone that’s not been brainwashed in our government controlled schools and can use his own brain
The relationship some people have with the Tory and Labour party is like a woman being in a abusive relationship with a Dickhead lad, always taking a beating and just as long as he said sorry and has promised never to do it again they get a second chance, again and again and again, first the Tory and Labour party steal and sell all our infrastructure with the biggest theft being our water industry and all the land that goes with it, then they go around the world murdering millions of totally innocent men women and children in our name, then they opened the doors to our country to replace us without asking anyone of us, they’ve even sold our young white girls out for votes, have you forgot about the way they treated the families of the 96 football fans, I could go on all day, what make me piss myself is the brainwashed still believe every word they say, you couldn’t make it up pmsl
All the fools always run off at this point because most of them have innocent blood on their hands
Chris Fairbrother Cuckoo!!!!!
Chris Fairbrother and it’s funny how these people will believe a NOVEL but not actual proven science!! Utter clowns
Al Freeman ho I’m i ? That’s why you have shit to say, some people don’t like the truth
Paul Hindley Never been proof of your so called god (note small ‘g’) so shut up sheep boy!!!
Paul Hindley Like you you mean!!!
Al Freeman is that the best you got ? And you wouldn’t say a word to my face you crank
Paul Hindley Just put your foil hat back on and sit quietly in the corner with David Icke!!!
Al Freeman there’s no blood on my hands as I’ve never voted for traitors, can you say that ? Now run along with your girlfriend the one that tagged you in
Paul Hindley And what has who I voted for got to do with the bullshit you are spouting??? And you my delirious friend have NO idea who I did actually vote for so BITE ME you god bothering, bullshit spouting idiot!! Go bathe in the blood of jesus or whatever crap you oddballs do…..
Paul Hindley You think I’d be scared of you???? Hahahaha! Shows how pathetic you are BOY!! Now just sit down and shut up like you were told!!!!
Al Freeman go away have you seen the state of you ? Go away
Paul Hindley Not a fucking sheep tho am I? You silly child lol!!!!!
Al Freeman it’s never been proven that viruses even exist, fact, it a money game, boy are you in for a shock when it all comes out in the coming weeks, you’ll also see what these traitors are that your supporting
Al Freeman 6 illegal wars and millions of totally innocent men women and children murdered in Tory and Labour voters names and not one shot fired at us first, you voted for this you clown, or is it OK because it’s not your family they’ve killed
Paul Hindley So come do tell….. Who/what did I, as in ME, vote for??? Let’s hear your wisdom?
Are you not in bed yet old man ? And your a Labour voter and do you know how I know this ? You think and also Labour party people do what you do and never say argue about what same one’s saying, Labour party voters just name calling, now go wash your hands and get to bed old man
Al Freeman On 12 April Dominic Cummings was seen in Castle Barnard during lockdown. Two days later, GlaxoSmithKline of Barnard Castle signed an agreement to develop and manufacture a Covid-19 vaccine with Sanofi of France. Dominic Cummings also sits in the PMs meetings with SAGE (Scientific Advisory Group for emergencies ). He therefore has access or input into the conversations in which Sir Patrick Vallance is Chief Scientific Advisor (whose previous employer was GlaxoSmthKline).
👉 This is WHY THE GOVERNMENT ARE DEFENDING HIM
– IMAGINE GETTING SACKED FOR DOING YOUR JOB lol
In 2012 GlaxoSmithKline were fined $3 billion for fraud, overcharging and making false claims about medicines in the USA. In 2016, GlaxoSmithKline were fined £37.6 million in the UK for bribing companies not to produce generic copies of their out of patent drugs, thus overcharging the NHS.
Despite the fines, these frauds were still massively profitable for GlaxoSmithKline. A perfunctory search on the company brings up similar frauds and fines it perpetrated in South Africa and India. All this within the last decade. I cannot find any information that anyone was jailed, or even sacked, for these criminal activities. It is absolutely astonishing that such an habitually criminal enterprise carries on serenely in the UK. And what is particularly interesting today is that it carries on its crooked activity from its massive manufacturing and research base in Barnard Castle, County Durham.
Paul Hindley So what you are saying is because of the way I voted that this is happening? And who the fuck mentioned that twat Cummings? I called you out because you are a science denying, bible bashing numbskull!!! I don’t give a flying shit about YOUR ‘politics’ just like you know fuck all about mine!!! So do the whole world a favour and STFU!!!!
I write a diary of what I have done each day there was a virus in March 1996 don’t know what
More bollocks
So there’s no such thing as a cold flu ect
Colds and flu are coronavirus
Pissing me off whatever it is
You can not keep letting this virus rule your life and getting paranoid be carful just get on with life it’s not killed millions just a drop in the ocean stop scaremongering
your position here is literally “I don’t know or care how quarantine works and I don’t care how many people die until it effects me personally”, which it inevitably will and then you’ll have the choice to learn empathy or nothing.
“We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.”
https://www.nejm.org/doi/full/10.1056/NEJMp2006372
Paul Hindley is quite right. Viruses are an invention of the Tory and Labour scum. You can ask anyone in Congo, Sierra Leone etc who lost relatives to the Ebola outbreak, for example. “Sir, I have no idea what you are talking about, please stop shouting and leave us alone”, they will tell you when you challenge their ridiculous claim that viruses are a thing that killed many local people. And that’s Congolese for “Fuck, you got me bang to rights, mate, I”m a tool of the Tory and Labour warmongers, long live 5G!”, as you can easily check with Google Translate. Ha! Wake up, sheeple!
I work in Air Conditioning and Ventilation of buildings and we have been quite busy trying to get the buildings of our clients back into use. Looks like I am going to be busy for quite some time then. 🤔🤔🤔🤔. We have some interesting data on the CDC model of how the spread started in Wuhan. I think it’s in the public domain.
Got this one? https://www.livescience.com/covid-19-did-not-start-at-wuhan-wet-market.html
Susan – Livescience is somewhat late to the party on that one! I made that point two months ago! Scroll down to the para on Wet Markets in this post: https://rectofossal.com/bat-country/
Actually I’ve seen more than one post, and Live Science have been good in keeping their information accessible… but I expect they have more traffic to keep up the information flow.
On 12 April Dominic Cummings was seen in Castle Barnard during lockdown. Two days later, GlaxoSmithKline of Barnard Castle signed an agreement to develop and manufacture a Covid-19 vaccine with Sanofi of France. Dominic Cummings also sits in the PMs meetings with SAGE (Scientific Advisory Group for emergencies ). He therefore has access or input into the conversations in which Sir Patrick Vallance is Chief Scientific Advisor (whose previous employer was GlaxoSmthKline).
👉 This is WHY THE GOVERNMENT ARE DEFENDING HIM
– IMAGINE GETTING SACKED FOR DOING YOUR JOB lol
In 2012 GlaxoSmithKline were fined $3 billion for fraud, overcharging and making false claims about medicines in the USA. In 2016, GlaxoSmithKline were fined £37.6 million in the UK for bribing companies not to produce generic copies of their out of patent drugs, thus overcharging the NHS.
Despite the fines, these frauds were still massively profitable for GlaxoSmithKline. A perfunctory search on the company brings up similar frauds and fines it perpetrated in South Africa and India. All this within the last decade. I cannot find any information that anyone was jailed, or even sacked, for these criminal activities. It is absolutely astonishing that such an habitually criminal enterprise carries on serenely in the UK. And what is particularly interesting today is that it carries on its crooked activity from its massive manufacturing and research base in Barnard Castle, County Durham.
Paul Hindley interesting.
Paul Hindley GSK’s HQ is not at Barnard Castle. It’s at Brentwood. Yes, they have just signed a collaboration with Sanofi so why don’t you contact the French media and tell them of your great conspiracy?
Dawn Vowles and very true
Gordon Millar they do have offices there !
Freda Heys I know. I’ve been there on numerous occasions. I used to sit on the Quality Management committee as a key supplier representative. There is absolutely NOTHING sinister about this. If any skulduggery was to be done, it would need umpteen Directors of both GSK and Sanofi and Cummings wouldn’t have a clue about formulating a vaccine so what would he be involved for? He would know anything about how they’re produced and he, like 99.9% of the population wouldn’t recognise a medical device if I rammed one up their backsides.This is just another nut job conspiracy theory. I’ve worked in the pharma/ biotech industry for 30+ years and I am sick to death of hearing about great big plots, Bill Gates being Dr Mengele reincarnated, 5G turning on viruses, how vaccines contain heavy metals and bovine fetal matter and all the other drivel.
Rectofussel Ambiguity. Would you care to identify yourself?
STOP LYING !
WE HAVE NEVER IN THE HISTORY OF INFECTIONS DISEASES QUARANTINED HEALTHY PEOPLE ! THERE ABSOLUTELY NO HEED FOR LOCKDOWN !
PROFESSOR DOLORES CAHILL IMMUNOLIST & MOLECULAR BIOLOGIST
They put every death as covid
but that’s childishly wrong.
quarantine has required uninfected people to limit their exposure since we found out that germs take time to make people sick.
I’m bored of this bullshit….
NEXT ..
Patrick James Irwin me too
The Flu Virus is still about so what, are you lot owing to hide away forever.👍👋🏴🇬🇧
Agreed bs virus
your position here is literally “I don’t know or care how quarantine works and I don’t care how many people die until it effects me personally”, which it inevitably will and then you’ll have the choice to learn empathy or nothing.
No..we are being lied to about the figures, CDC just admitted it. Italy admitted it,etc
20th next month we need the gov. To repeal the emergency laws that were brought in, if they dont then we know its a con.
Mick Levoir
We know already 👍
Mick Levoir why would you say that out of interest?
Piss off spreading this Government Corona Bullshit !😠
It means we’ve been lied to again
Worrying
Utter shit question
If no vaccine is found people will have to get used to living with it .
Stuart Mcilmoyle we have to live with flu ????
Meta Connolly aye that’s true , I mind when hiv came on the scene , no vaccine but we leaned to live with it . So hopefully we get one.
Wow! You really triggered the moonfruit this time. Kudos!
David – it appears my circle of upset has extended beyond the antivaccine mob! I also think there’s scope for another PhD in examining whether those of us who’ve directly observed viruses have been suffering a mass psychogenic illness for 80 years…
Rectofossal Ambiguity And they walk among us… ScienceNews, which I’ve often visited, shut down their comments some months ago. Basically anything involved with evolution, climate change or vaccination was just pounced upon by these fruitloops, and no actual comment or discussion was possible. Viz used to have a feature by “The bloke down the pub – Britain’s least well-informed commentator”. Turns out to have been a predictions rather than a joke 😱💩🚽
Is fruit loop a technical term here 🤣🤣🤣🤣🤣🤣🤣
Sandy JP Borrowed from the Yanks!
BTW, I don’t know why we link fruit to these barmpots – there’s “fruitcake” as well!
Sooner they get a vaccine the better no more doom and gloom fingers crossed
Rosalyn Goward Yeah I’m not having that Democratic garbage injected into me
Yes it will as long as you report the facts and not this bs
Stop this B.S now my neighbour has hhad people in most days through whole lockdown in uk partys most weekends as well kids in property and a member of bame community so by now they shouldve shut up but havent they still going so stop this B.S and lies u want ppl to commit suicide as cant c end to the torture of noise thats gone on for months constantly
Worth a read
LMFAO…. coronavirus the new Terrorism. what an obvious False Flag .
Invisible threat.
create Fear
Control population.
…..911 in every country, and no buildings demolished.
The Hospitals are QUIET.
Non C9v1d deaths are being counted as C9v1d.
People talking. We are sick of this scam.
Gordon McCulloch You believe what you want to believe. This virus is real and common sense should prevail.
Oh my dear some are sold on the fearc
They are using this virus to get you into habits which will eventually lead into loss of privacy and freedom. Know the truth.
Conan Wortley yawn- another conspiracy theorist! So what killed the 37,000 people then??
Lesley Garton do you know where the word conspiracy theorist came from. If not read up..
I’d rather be 1 of those than blind to the truth 😁
Same stats as seasonal flu, remember people have been dying because they have underlying issues, they are even cooking the books. Don’t believe everything you are told by government. Question everything.
The CIA
The only time it’s a theory though is when it’s not true
your position here is literally “I don’t know or care how quarantine works and I don’t care how many people die until it effects me personally”, which it inevitably will and then you’ll have the choice to learn empathy or nothing.
I’m 60, heart and other issues, but since I know the truth about this so called virus.. it does not exist, it’s every body else who is acting as though Boris Johnson is their saviour. Please people question everything.
Conan Wortley And every Leader in every Country in the World?
Chinese, N Koreans.
Payback 🤫
https://youtu.be/NcEeBCPsOmI
Well if bojo followed the rules at the beginning it wouldn’t of got this far oh yeah TORIES dont follow the rules
Pauline Finch bullshit
Fuck off with this utter BS.
Reported as FALSE NEWS.
SCAMdemic.
Fear has the moist robots dying to be saved from the inevitable, someday we are all going to die, but the robots will never truly live.
More oil please vicar, the limbic system has caused a problem in tbe cortex.
What a load of bollocks. Only if the Chinese get to release more “accidents” onto the world (to make massive economic capital), much easier than conventional war & much more profitable. Especially when several multi billionaires control the media & the (crap) scientific advice & modelling. They have lots of interest in testing, vaccines & a society like China where they can make lots of money by controlling people & having lots of incredibly cheap labour with few human rights.
The people who want lockdown to end are the same people taking guns to the store in case a yogurt looks at them funny… are you ill?
Stockholm syndrome …. see a doctor
A goverment paper on19 March classified this as not being a High Consequential Infectious Disease…….and then house arrest came in .aka lockdown….and the programme has to be followed through…the global script
House arrest isn’t “lockdown” and the reclassification was to deprive small business of the insurance payouts they should have been entitled to….
Claire Myers defo 100%house arrest
No it wont to many braindead selfish peoplw and a useless Pm
Stay alert, stay safe, keep washing hands, stay 6 FEET apart
Georgia Erskine
If it mainly spreads “inside buildings” then what the actual fuck are you doing locking yourself inside a bloody house??? Are you demented or something? Logic taken a back seat to idiotic ideals and idea’s??? QUIT BEING A TOTAL ARSEHEAD!!!
Laughed out loud at this one. Kudos to you, Dr. Gekneeus. With that perfect “no deal” logo as well, it’s teasingly suggestive of a master of satire. But every day brings new waves of comments that at first look like satire but turn out to be orders of magnitude dumber and thus probably genuine.
They say that the average person (the median, to be precise) is as thick as pigshit and half the population are even thicker than that. It would be interesting to know how the distribution looks if you restrict it to BTL commenters on evolution/climate/health/vax blogs. My guess is strongly bimodal, and back in the day natural selection would have taken care of one of the modes. Pandemics aren’t nearly as surgically precise, unfortunately, although the huge number of C-19 cases among maskless, hymn-singing congregations of religious lunatics in the US who think Jesus will protect them is at least an encouraging sign of some specificity.
No need to panic.
To anyone that still believes this hoax 🐑 Baaaaaaaaaaa
Just like the flu will never go away
Absolute codswallop.
Not if the Democrats get control this will be the new normal
Same 💩 different day! Virus? No virus? I know what I believe
Oh shut up. This is a crock.
If anyone thinks lockdown is a right pain just wait till Brexit, you’ll be facing longer supermarket queues for bread rationed to five slices each and sweet all else on the shelves 😕
Tim Rome bullshit
Tim Rome Ha ha ha ha ha ha ha
This is all about Democrats control over America.
No more lockdowns are coming until the NWO is in full worldwide power.
Stop stirring things up !
Yes….when liberals and democrats are defeated👍👍👍
The most depressing load of garbage I have read for a long time. If I believe this, it’s time to dig a big hole and jump in and stay there… But then, maybe I could stay alive for ever…
More bullshit
Give it up! After these riots, no masks, no social distancing…. this ship has sailed!
Sounds like a life not fit for humans
A University of Oxford professor who produced a competing model to the “apocalyptic Imperial College model” (UnHerd theory) said there’s a chance that doing nothing would’ve been a more effective COVID-19 response than the various lockdowns implemented around the world.
https://bit.ly/2A16zxQ
It was a stupid mistake to have ever allowed this “UnHerd” nonsense that is posing as science to have happened at all.
“The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history” – Denis G. Rancourt, PhD
https://www.researchgate.net/publication/340570735_Masks_Don't_Work_A_review_of_science_relevant_to_COVID-19_social_policy
Ramiro – this is utter, utter bollocks, I’m afraid. It’s written by a climate change denying conspiracy theorist (nice ad hom there) in an essay that cherry picks studies which he clearly does not understand, let alone is able to critically evaluate.
He sets his position out early: “The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.”
That’s not the opening to a scientific review, that’s a political manifesto.
Without doing a deep dive on all 42 studies here’s a representative example:
“We identified 6 clinical studies … In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
That paper (https://www.cmaj.ca/content/188/8/567) was looking at the difference in levels of *protection* between N95 and surgical masks. He thinks it’s saying neither works – or he’s deliberately taking a sentence out of context and relying on people not looking at what he’s citing.
This is an individual with an agenda using his credentials in physics to make a political argument. But he has no qualifications in the biological or biomedical sciences – and it shows.
Rectofossal Ambiguity “The relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective-dose is smaller than one aerosol particle" – Denis G. Rancourt, PhD
Rectofossal Ambiguity A University of Oxford professor who produced a competing model to the “apocalyptic Imperial College model” (UnHerd theory) said there’s a chance that doing nothing would’ve been a more effective COVID-19 response than the various lockdowns implemented around the world. https://bit.ly/2A16zxQ
Rectofossal Ambiguity ‘Scaring people into obeying’: Brit Hume shares COVID-19 findings from Nobel prize-winning scientist contradicting lockdowns
https://twitchy.com/samj-3930/2020/05/03/scaring-people-into-obeying-brit-hume-shares-covid-19-findings-from-nobel-prize-winning-scientist-contradicting-lockdowns/?utm_content=buffer915af&utm_medium=social&utm_source=facebook.com&utm_campaign=buffer&fbclid=IwAR0zSY3fYYgSg1-76qt5_9sx64VjcWsczCuPcKauSq2QantjQPW4pPAVJJA
Rectofossal Ambiguity Senator Rand Paul pushes back on Dr. Fauci’s claims there is no evidence of immunity, and boldly questions the modeling used while pointing out there have been more people wrong with these models than have been right.
Senator Rand Paul also points out something that is hardly ever been discussed in main-stream and social medias, the Lockdowns or “UnHerd” method are a result of Neil Ferguson’s Imperial College model which received a very public rebuke from Leading Swedish Epidemiologist Johan Giesecke, a sentiment that is being echoed by others including veteran of Epidemiology Dr. Knut Wittkowski and countless field doctors and physicians. https://youtu.be/uArJ9Ye1Ueo
Rectofossal Ambiguity “A Swedish professor who was the State Epidemiologist for Sweden between 1995 to 2005, then served as the first Chief Scientist of the European Centre for Disease Prevention and Control (ECDC), “blasted” Professor Neil Ferguson, the British epidemiologist from the Imperial College London, who wrote a paper that convinced many countries, including the United States, Germany, France, and those in the United Kingdom, to impose lockdowns to deal with the coronavirus”
Asked whether European countries instituting a lockdown to deal with the coronavirus was a misguided policy and whether it was doing more harm than good, he answered that he was worried about politicians assuming dictatorial powers: “Yes. I think so, on the whole.
https://www.facebook.com/100003687006865/posts/1910558635743685/?d=n
stop being part of the problem and be a part of the solution.. this fear porn bullshit is not part of the solution.. there is plenty of evidence to counter the narrative.. but i’ll throw you a few clues
1. research the PCR test kits, their reliability, who has the monopoly on them
2. Neil Fergusson and his Magical Antiquated Modelling Machine (MAMM) and his fake numbers which the whole world bought but opted to ignore the imperial colleges adjustment to 25k in the UK.. no media outlet picked this up and look at the result?
3. patents going back to 2003 from the CDC/NIH.. google USA Government Oversight vs. Dept of Health
4. the thousands of drs, nurses, profs, former nobel prize winners, etc coming forward only to be smeared as they are providing actual evidence
5. Japan..850 total deaths and no draconian measures..huh?
6. Covid Alert #2 (Mar 24) and Covid Alert #3 (Apr 3rd or 4th). Plus the head of Chicago Dept of Health stating on tv that all deaths are listed as COVID deaths.. yeah more fear porn..
and much much more.. sadly, everyone is too focused to research deeper thanks to the latest false flag/psyop and now i’m seeing this spam crap on my feed..
I guess you should re-think you social media marketing strategy..
“Fauci predicts another coronavirus outbreak in fall 2020!”
Actually, according to veteran scholar of Epidemiology Dr. Knut Wittkowski, Fauci all but guaranteed an outbreak will in fact happen.
“However, if we are preventing herd immunity from developing, it is almost guaranteed that we have a second wave as soon as either we stop the social distancing or the climate changes with winter coming or something like that,”
https://www.facebook.com/100003687006865/posts/1908194622646753/?d=n
“The Rockefeller University releases statement concerning Knut Wittkowski
April 13, 2020
“The opinions that have been expressed by Knut Wittkowski, discouraging social distancing in order to hasten the development of herd immunity to the novel coronavirus, do not represent the views of The Rockefeller University, its leadership, or its faculty.
Wittkowski was previously employed by Rockefeller as a biostatistician. He has never held the title of professor at Rockefeller.”
https://www.rockefeller.edu/news/27872-rockefeller-university-releases-statement-concerning-dr-knut-wittkowski/
Enough with this bullshit already. The majority know the truth about this “virus” so what did you want out of this? Fear mongering? Shove it.
have quarantine of the pat ended?
did you do even 5 minutes googling before writing this article?
Oh dear oh dear. This increasingly unhinged comments section shows exactly why humans are now in such deep shit.
Herds of pig-ignorant nutjobs have become convinced by years of exposure to right-wing media (and each other) that experts in medicine, epidemiology, climate science, you name it, are all part of a vast conspiracy of lies, and that only pig-ignorant nutjobbery possesses The Truth(TM).
It took decades to get here, to this sub-QAnon level of stupidity, and it’d take decades to get back to having a more-or-less educated populace with just a few nutters, even if we started now. And there’s no sign of us starting any time soon, but every sign of it getting worse.